Have you ever been asked by clients “How painful is the surgery going to be?” Almost every time! An invasive procedure involves incising the skin, subcutaneous tissues, muscles, manipulation of organs, sometimes incision on organs and suturing every layer back. Each step is a pain stimulating action, be it an abdominal surgery, orthopedic procedure, eye surgery or thoracic surgery. Pain is ubiquitous across species, breeds, sex and age. It is a misconception that neonates do not feel pain, cats have higher pain tolerance and so on.
Few terms you should keep in mind1,6:
- Noxious stimulus- Any stimulus which causes or can potentially cause tissue damage.
- Nociception and pain- Nociception is the unconscious response of nervous system to a noxious stimulus while pain is the unpleasant sensory and emotional experience due to a noxious stimulus. Simply put, the reflex of withdrawing your arm after it touches a warm vessel is nociception. The unpleasant feeling and urge to take care of the burn and not touch the vessel again is pain.
- First pain- The sharp sensation of pain which can be localized accurately. E.g. Pin prick on finger tips.
- Second pain (True pain)- It is the severe itch to agony or burning aching pain which is lower in intensity than first pain but lasts longer. It occurs due to inflammatory mediators from the damaged tissue.
- Hyperalgesia- It is an exaggerated response to noxious stimulus due to lower pain threshold, commonly seen in spinal injuries.
- Referred pain- Pain sensation felt in a body part other than the site of injury. E.g. Elder dogs tend to bite their paws who have arthritic changes in joints.
- Phantom pain- It is the pain brain perceives in the body part after its removal from the body. E.g. Limb amputation.
- Acute pain- It is elicited from a specific cause and is short lasting.
- Chronic pain- It is the pain which extends beyond the expected period of healing. The duration varies from days to months to years.
Analgesia is an integral part of anesthesia. Without adequate pain management, surgical pain is insufferable for our patients. It is vital to understand how pain is elicited in the body. Nerves pass on messages to each other in the form of nerve impulses which run down from brain to spinal cord through millions of neurons till it reaches the effector organ and from receptor organ through neurons, to the spinal cord and finally to the brain. Pain impulses traverse in the similar manner. The nerve route which conducts pain impulses to and from the brain are called pain pathways. Let us understand how pain pathways operate.
Pain impulse conduction is divided into five stages:
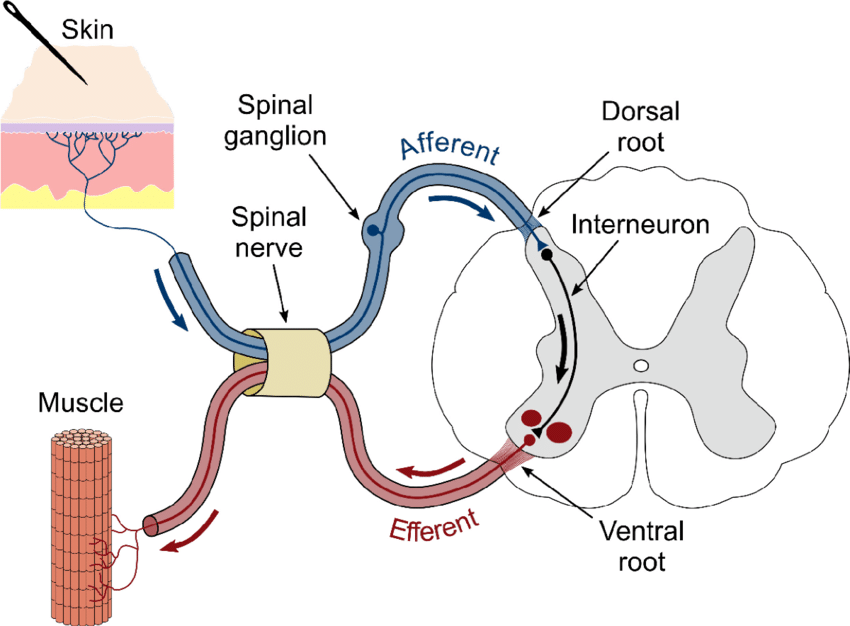
1. Sensory pathway to the spinal cord:
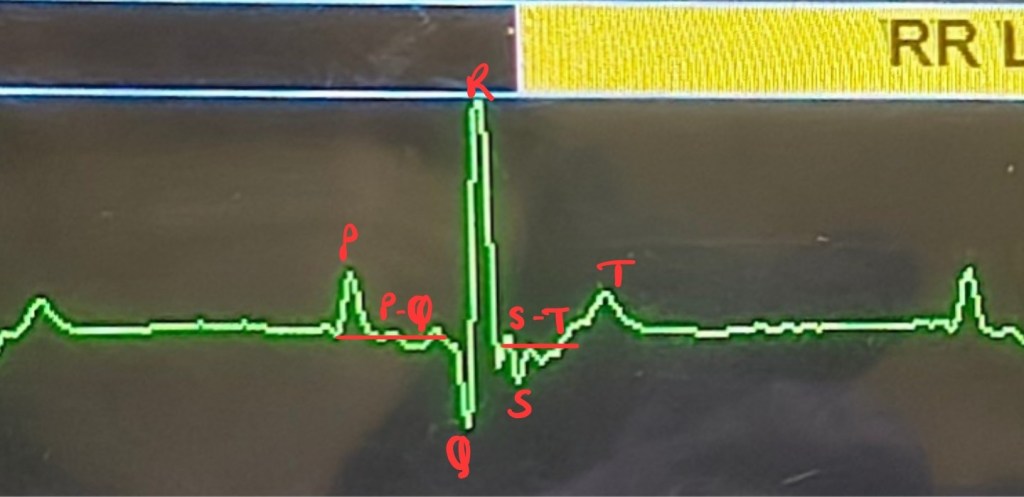
Each organ, muscle, fascia, skin, mucus membranes, connective tissues, ligaments, periosteum, bones, tendons and arterial vessels are enervated with pain receptors/nociceptors which are sensory in nature1 Nerves which carry impulses from receptors to the brain are sensory nerves. These receptors convert a painful physical or chemical stimulus into an action potential. Nociceptors respond to heat, pressure, vibrations and inflammatory cytokines. Pain impulse from nociceptor is carried to the spine via afferent nerve6.
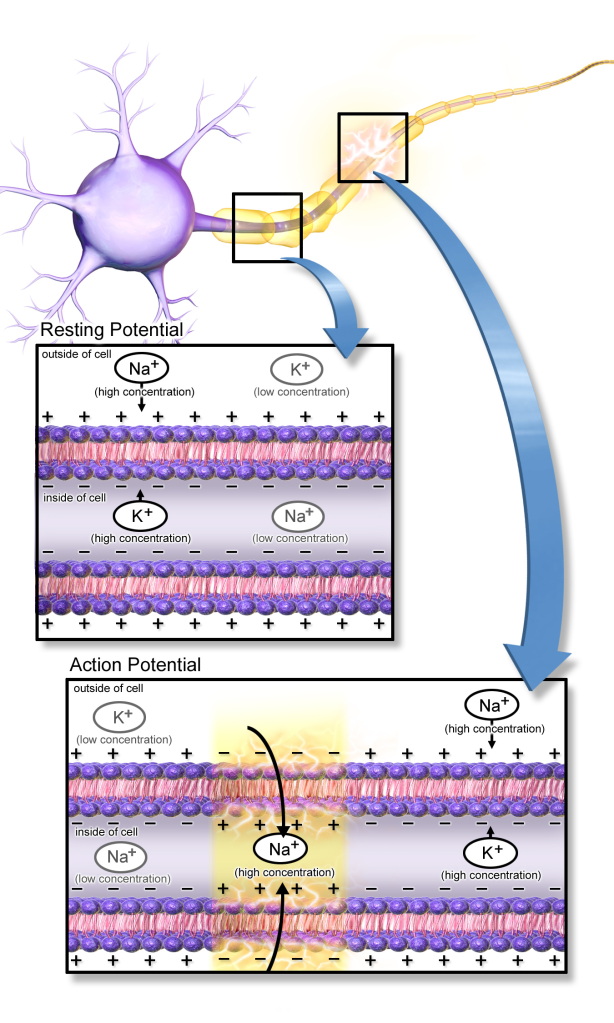
When a stimulus acts on the skin, it activates a stimulus gated ion channel, there is an influx of sodium or calcium ions, which traverse a diffusion gradient. This leads to depolarization of the plasma membrane and an action potential is generated6,9.
2. Processing of pain in the dorsal horn of spinal cord:
The pain impulse enters the spine through axon of the afferent nerve from the dorsal horn grey matter. Once the impulse enters the spine, neurotransmitter is released which is proportionate to the strength of the original stimulus. The neurotransmitter can either be excitatory or inhibitory in nature, which either amplifies or inhibits the pain impulse, respectively. Grey matter in the spinal cord is divided into ten laminae (Rexed’s laminae I-X), off which the afferent nerve has input in laminae I to VI where pain impulses are processed1. Axons of these afferent nerves synapse with efferent nerves which carry the pain impulse to the brain6.
3. Ascending tracts to the brain:
Thalamus is the centre of pain processing in the brain. Efferent nerves exit from lamina I and deeper laminae of the dorsal horn of spinal cord to the thalamus (spinothalamic tract), specifically the caudal part of the ventral medial nucleus6.
4. Processing of painful stimuli in the brain:
From the thalamus, the pain impulse goes through divergent pathways:
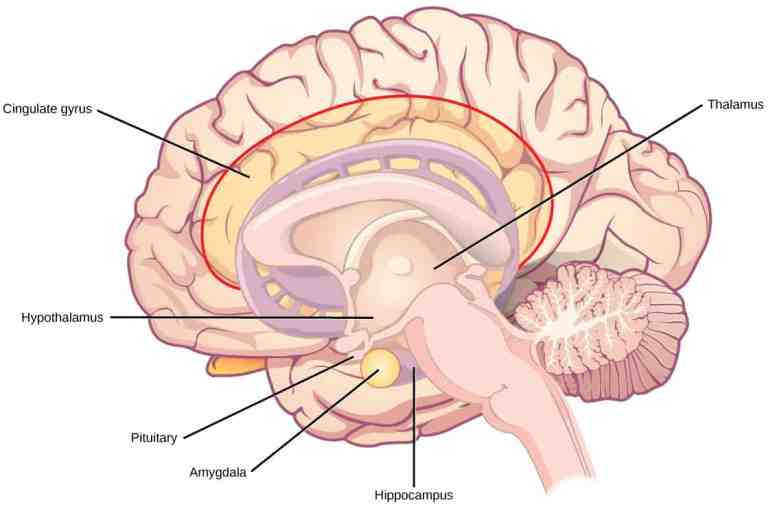
SI Somatosensory cortex- This helps the body differentiate the elements of pain. Whether the pain is due to touch from a sharp or blunt object, if the object is warm or cold, if it is solid or liquid in nature, shape/texture of the object and so on6.
SII Somatosensory cortex- It is involved in recognition, learning and storing memory of pain6, which is responsible for our “painful experience”.
Insular cortex- Involved in the autonomic responses to painful stimuli8 by stimulating the sympathetic and parasympathetic nervous systems, like increasing heart rate while watching a horror movie, or rapid breathing after a fall.
Anterior cingulate gyrus- Involved in the behavioural response to pain6. Simply speaking, it helps us learn from our past painful mistakes. Thought of covering your eyes during horror scenes or fast forwarding it entirely, or thinking to walk slow where you fell last time. It is your “inner voice” which tells you to not make bad decisions.
5. Descending analgesic pathway11:
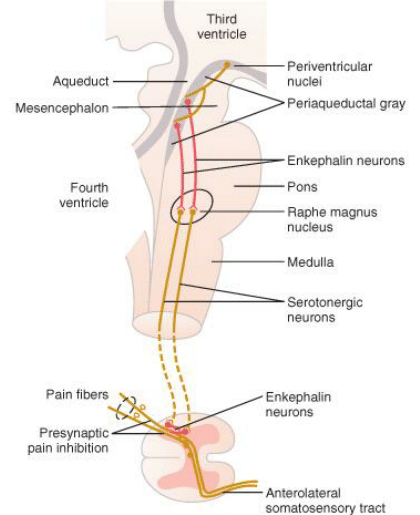
Once the brain learns from the anterior cingulate gyrus about the response to the pain, dopaminergic neurones projected from substantia nigra release dopamine in the basal ganglia. Dopamine has an analgesic effect6. Basically, it executes the decision taken by the anterior cingulate gyrus and protects the body from painful stimulus. Literally covering your eyes when the horror scene plays, or watching every step you take in the fall-zone.
Pain killers made by the body
Mammalian body is capable of pain management, to some extent. Pain pathways themselves secrete neurotransmitters and neuromodulators which counter pain stimuli.
γ-Amino butyric acid (GABA), produced in lamina II of spinal cord grey matter, inhibits calcium ion influx and stops release of excitatory neurotransmitters, before the pain impulse can stimulate the efferent nerve5.
Enkephalin is an opioid peptide which reduces release of excitatory neurotransmitters by inhibiting calcium channels in afferent nerves3, thus slowing down the pain impulse transmission. Endorphins, Dynorphins and Endomorphins are other opioid peptides which modulate pain transmission when released with excitatory neurotransmitter, Glutamate. Endorphins and Enkephalins act on opioid receptors (µ, δ and ĸ) to reduce anxiety2.
Somatostatin and Glycine have inhibitory effect on the dorsal horn of the spinal grey matter6.
How do pain killers work with pain pathways?
Non-steroidal anti-inflammatory drugs (NSAIDs)- Cyclooxygenase (COX-2) is an enzyme which is involved in the formation of prostaglandins. Prostaglandins intensify the sensation of peripheral pain by lowering the threshold of generation of action potential in afferent nerves and inhibiting action of glycine in the spinal cord. NSAIDs inhibit formation of COX-2 and reduce the formation of secretion of prostaglandins7.
Opioids- µ receptors are present in abundance in the periaqueductal region (origin of the descending analgesic pathway) (Image of periaqueductal region). When activated these receptors secrete neurotransmitter GABA and inhibits pain impulse transmission4.
N-methyl- D aspartate receptor antagonist- NMDA receptors in the spine are blocked by drugs like Ketamine (NMDA antagonist) and inhibit excitatory neurotransmitter- Glutamate to stop depolarization of nerve membrane6.
α2 agonists- Binding of catecholamines to α2 receptors hyperpolarizes the spinal neurones and inhibits neurotransmitter release from afferent nerves6. α2 agonist drugs, like Xylazine and Dexmedetomidine, help with binding of more catecholamines with α2 receptors and thus, reducing pain impulse.
Sodium channel blockers- Local anesthetics block selective sodium channels which propagate the action potential induced by painful stimulus. Inhibiting influx of sodium ions into the nerve membrane does not depolarise the afferent nerves and pain impulse is not generated6.
Knowledge about various aspects of pain pathways helps us understand how pain is elicited and choose appropriate analgesic drugs for each surgery patient and modify anesthesia protocol, if required. It eventually improves surgical outcome, faster recovery and healing.
Connect with me on LinkedIn and Instagram. Subscribe to the AnesWise newsletter for future content notifications. Kindly leave a feedback as it helps improve the blog. Feel free to ask your doubts in the comment section or email it to dr.sahilmehta@outlook.com
Edited by Prajakta Alase
Citations:
- Almeida, T.F., Roizenblatt, S. and Tufik, S., 2004. Afferent pain pathways: a neuroanatomical review. Brain research, 1000(1-2), pp.40-56.
- Koneru, A., Satyanarayana, S. and Rizwan, S., 2010. CURRENT KNOWLEDGE AND FUTURE TRENDS OF ENDOGENOUS OPIOIDS: THEIR PHYSIOLOGICAL ROLE AND RECEPTORS.
- Li, H., Wu, L. and Li, Y.Q., 2003. Opioid peptides modulate the response of neurons of the superficial laminae of the rat spinal dorsal horn to GABA. Biochemical and biophysical research communications, 307(3), pp.730-736.
- Liao, D., Lin, H., Law, P.Y. and Loh, H.H., 2005. Mu-opioid receptors modulate the stability of dendritic spines. Proceedings of the National Academy of Sciences, 102(5), pp.1725-1730.
- Lu, Y. and Perl, E.R., 2003. A specific inhibitory pathway between substantia gelatinosa neurons receiving direct C-fiber input. Journal of Neuroscience, 23(25), pp.8752-8758.
- Meintjes, R.A., 2012. An overview of the physiology of pain for the veterinarian. The Veterinary Journal, 193(2), pp.344-348.
- Seibert, K., Zhang, Y., Leahy, K., Hauser, S., Masferrer, J., Perkins, W., Lee, L. and Isakson, P., 1994. Pharmacological and biochemical demonstration of the role of cyclooxygenase 2 in inflammation and pain. Proceedings of the National Academy of Sciences, 91(25), pp.12013-12017.
- Woolf, C.J., 2004. Pain: moving from symptom control toward mechanism-specific pharmacologic management. Annals of internal medicine, 140(6), pp.441-451.
- Blausen.com staff (2014). “Medical gallery of Blausen Medical 2014”. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. – Own work, CC BY 3.0, https://commons.wikimedia.org/w/index.php?curid=29452220
- https://human-memory.net/cingulate-cortex/
- https://www.researchgate.net/figure/Descending-analgesic-pathway-from-mesencephalon-through-brainstem-to-spinal-cord_fig1_45677305
- https://i0.wp.com/www.naturphilosophie.co.uk/wp-content/uploads/2016/06/Pain_Symbolised_Cartoon.jpg?ssl=1




Leave a reply to The Mindful Migraine Blog Cancel reply